| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Original Article
Volume 4, Number 1, February 2014, pages 17-22
The Effectiveness of Focused Assessment With Sonography for Trauma in Evaluating Blunt Abdominal Trauma With a Seatbelt Mark Sign
Scott R. Kelleya, d, Betty J. Tsueib, Andrew C. Bernardc, Bernard R. Boulangerc, Paul A. Kearneyc, Phillip K. Changc
aDepartment of Surgery, Good Samaritan Hospital, Cincinnati, Ohio, USA
bDepartment of Surgery, University of Cincinnati, Cincinnati, Ohio, USA
cDepartment of Surgery, University of Kentucky, Lexington, Kentucky, USA
dCorresponding author: Scott R. Kelley, Department of Surgery, Division of Colon and Rectal Surgery, Good Samaritan Hospital, TriHealth, 379 Dixmyth Avenue, Cincinnati, Ohio 45220, USA
Manuscript accepted for publication December 3, 2013
Short title: The Effectiveness of FAST
doi: https://doi.org/10.14740/jcs207w
| Abstract | ▴Top |
Background: Specific injury patterns have been recognized from seatbelt use including hollow viscous, mesenteric, and musculoskeletal injuries. We aimed to evaluate if focused assessment with sonography for trauma (FAST) is a reliable screening tool for the initial evaluation of the blunt abdominal trauma patient with a seatbelt sign.
Methods: A retrospective review of adult trauma patients with blunt abdominal trauma and a positive seatbelt sign were evaluated over a three-year period. Data collected included age, gender, Glasgow coma scale (GCS), presence or absence of abdominal tenderness, results of diagnostic studies, operative findings, missed injuries, and mortality.
Results: A total of sixty-nine patients were evaluated. Fifty-eight ultrasound scans were interpreted as negative and 11 positive. Three of the 11 were taken immediately to the operating room. The remaining 8 underwent computerized tomography (CT) according to protocol and clinical management was altered in two. Sixteen patients with a negative ultrasound examination underwent CT. Our series revealed 11 true and no false positives, as well as 54 true and 4 false negatives. The sensitivity of utilizing FAST for detecting a clinically significant injury in this study is 73% with 100% specificity, a negative predictive value of 93%, positive predictive value of 100%, and accuracy of 94%.
Conclusions: The use of FAST, not as a single diagnostic modality, but as a screening tool with selective use of CT, is a relatively reliable instrument for the initial evaluation of the blunt abdominal trauma patient with a seatbelt mark sign.
Keywords: Blunt abdominal trauma; Seatbelt sign; Computed tomography; Sonography; Screening; Fast; Sensitivity; Specificity
| Introduction | ▴Top |
Three distinct forces occur during a motor vehicle collision. The first is the force of the automobile colliding with another object. The second is the force of the unrestrained occupant colliding with the interior of the vehicle. The third is the force of the internal organs colliding against the body’s musculoskeletal structures, which often results in serious or fatal injuries.
A seatbelt functions to stop the occupant with the automobile, preventing the body from continuing to travel at the vehicle’s primary speed after it has stopped, thus eliminating the second force of a vehicular collision. The properly worn safety belt is designed to spread the rapid deceleration energy over the larger and stronger parts of the body; namely the pelvis, chest, and shoulders.
The protective effect of safety belts in reducing morbidity and mortality from vehicular accidents has resulted in widespread legislation mandating their use. Seatbelts have decreased both the overall fatality rate in motor vehicle collisions as well as the severity of non-fatal moderate to critical injuries [1, 2].
Although seatbelts greatly decrease the associated morbidity and mortality of automobile collisions, specific injury patterns have been recognized as arising directly from their intended use including hollow viscous, mesenteric, and musculoskeletal injuries [3-6]. Seatbelt related injuries are the result of the altered physics of rapid deceleration caused by restraint with the lap belt and shoulder harness. Injury from seatbelts, and the associated seatbelt syndrome, was first introduced by Garrett and Braunstein in 1962 in which they described a variety of injuries associated with the lap belt restraint [7]. An abdominal seatbelt mark sign is classically described as abdominal wall contusions and abrasions resulting from a seat restraint. Seatbelt syndrome consists of a seatbelt mark sign as well as the underlying mesenteric, visceral, and musculoskeletal injuries.
The University of Kentucky trauma service began using ultrasound scans in 1996 as a screening tool for the evaluation of trauma patients. Prior to that time all patients requiring objective non-operative evaluation of the abdomen received a computerized tomography (CT) scan or underwent diagnostic peritoneal lavage (DPL). After instituting a focused assessment with sonography for trauma (FAST) screening algorithm (Fig. 1) CT was used more selectively and DPL was rarely utilized. Most blunt abdominal trauma patients seen at the University of Kentucky with a seatbelt sign are evaluated using an ultrasound based protocol. A study conducted at the University of Louisville concluded that FAST is an unreliable method for assessing intraabdominal injury in patients with seatbelt marks [8]. We aimed to evaluate our hypothesis that the use of FAST, not as a single diagnostic modality, but as a screening tool with selective use of CT, is a relatively reliable instrument for the initial evaluation of the blunt abdominal trauma patient with a seatbelt sign.
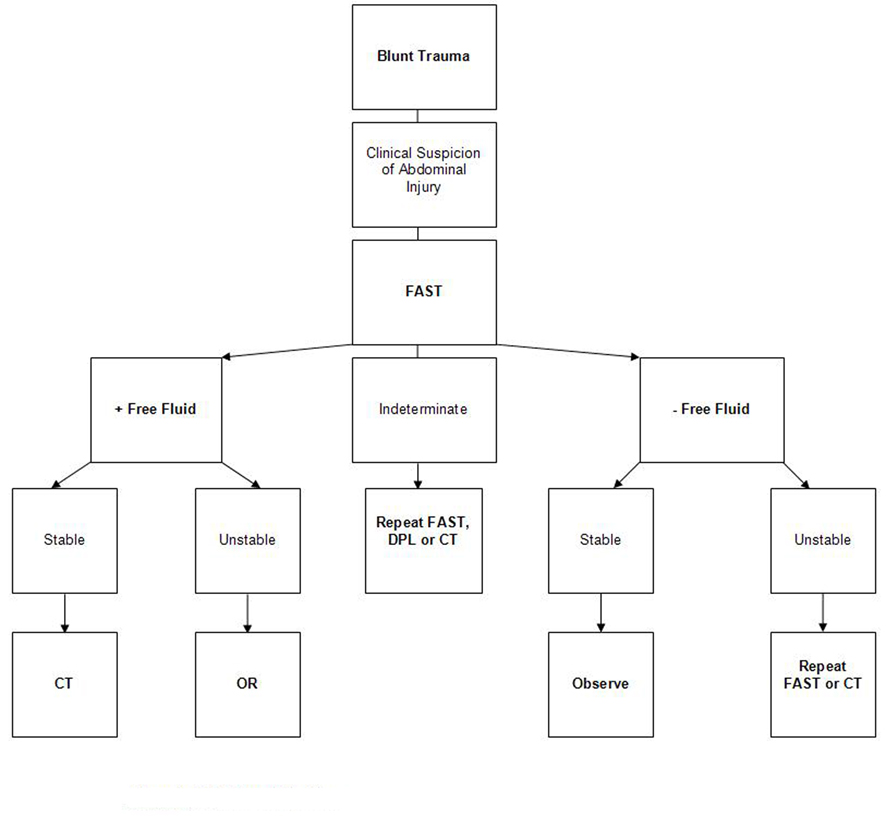 Click for large image | Figure 1. FAST based algorithm. |
| Methods | ▴Top |
After obtaining approval from the University of Kentucky Institutional Review Board (IRB), a retrospective review of adult trauma patients (≥ 18 years of age) with blunt abdominal trauma and a positive seatbelt sign were evaluated by the trauma service at the University of Kentucky over a three-year period. Data collected included age, gender, Glasgow coma scale (GCS), presence or absence of abdominal tenderness, results of diagnostic studies (ultrasonography and CT), operative findings, missed injuries, and mortality. All ethical guidelines for conducting human studies were followed according to the University of Kentucky IRB.
Ultrasound scans were performed in a standard manner and interpreted by the attending trauma surgeon and/or fellow. Evaluation included pericardial, hepatorenal, splenorenal, and suprapubic images. Results were interpreted as positive if free fluid was present in one or more of the viewable areas evaluated and negative in the absence of free fluid. If a definitive interpretation could not be made the result was recorded as indeterminate. FAST imaging was carried out using a Philips ATL 3,500 machine with a variable frequency transducer (Philips Medical Systems, Bothell, WA).
For the subset of patients requiring CT as part of their assessment, an abdominal and pelvic CT scan was performed after administration of oral and IV contrast using a Siemens multislice CT scanner (Siemens Medical Systems, Malvern, PA). Staff radiologists along with either the attending trauma surgeon and/or fellow interpreted the CT scan results.
| Results | ▴Top |
At total of one hundred and three blunt abdominal trauma patients who presented with a seatbelt sign were evaluated. Thirty-four were excluded (16 less than eighteen years of age, 6 transferred to our facility after CT was performed, 8 evaluated with CT only, 4 evaluated with observation alone) leaving an aggregate of 69 patients who received FAST as part of their initial evaluation.
Of the 69 patients included in our study the average age of our patient population was 46.6 (range 18-80) with a nearly equal number of females (n = 35) and males (n = 34). Most were neurologically intact with sixty-two (90%) presenting with a GCS of 15, four (6%) with a GCS of 14, and one each (1%) with a GCS of 13, 12, and 3T. Abdominal tenderness was noted in a total of 44 (64%) patients. Two (3%) patients died, both secondary to multiorgan system failure. One (80 years old) presented with a GCS of 3T and the second (79 years old) presented with a GSC of 15. Both had negative FAST exams, did not undergo subsequent abdominopelvic CT scanning, and neither were operated on. The remaining 67 patients (97%) were all eventually discharged from the hospital.
Fifty-eight (84%) ultrasound scans were interpreted as negative and 11 (16%) positive. We did not have any indeterminate examinations. Three of the 11 interpreted as positive were taken immediately to the operating room for instability, with all having mesenteric or gastrointestinal tract injuries requiring resection. The remaining 8 stable patients underwent CT (within 15 to 140 minutes) according to protocol and clinical management was altered based on the CT findings in two. Both underwent exploratory laparotomy with a grade 1 liver laceration found in one and a jejunal perforation and sigmoid serosal injury in the other (Table 1). Sixteen of the 58 patients with a negative ultrasound examination underwent a CT scan (within 15 minutes to 13 hours) secondary to abdominal pain (11) or instability (5), of which 12 were negative for intraabdominal injury. Two splenic injuries lacking abdominal pain were treated non-operatively, one colonic serosal tear and jejunal perforation with associated abdominal pain required repair, and one with multiple sigmoid mesenteric lacerations and serosal tears coupled with abdominal pain required operative intervention (Table 2). Our series revealed 11 true and no false positives, as well as 54 true and 4 false negatives. The sensitivity of utilizing FAST for detecting a clinically significant injury in this study is 73% with 100% specificity, a negative predictive value of 93%, positive predictive value of 100%, and accuracy of 94%.
 Click to view | Table 1. True Positive Results |
 Click to view | Table 2. False Negative Results |
| Discussion | ▴Top |
In the critically injured patient accurate diagnosis and prompt treatment of life-threatening injuries are crucial to survival. Other than physical examination different investigative modalities such as DPL, CT, and ultrasonography can be utilized in the evaluation of the blunt abdominal trauma patient with a seatbelt mark sign. Physical examination alone can be subtle and unreliable in a polytrauma patient and has been shown to be relatively poor for diagnosing intraabdominal injury [9].
DPL, although not performed in our study, is rapid, inexpensive, can be performed at the bedside and utilized in hemodynamically unstable patients, and is relatively safe. DPL has an overall sensitivity of 98%, specificity of 98%, and diagnostic accuracy close to 100% [10]. Criteria specifically designed to help aid in the diagnosis of hollow viscus injuries utilizing fluid measurements of amylase, alkaline phosphatase, and white blood cell to red blood cell ratios have shown high diagnostic sensitivity and specificity [11, 12]. DPL is an invasive exam, does not identify the cause of hemoperitoneum, and a positive study may lead to a non-therapeutic exploratory laparotomy [13].
In the hemodynamically stable patient abdominal and pelvic CT is useful for evaluating both intra and extraperitoneal (retroperitoneum, thoracic, pelvic) injuries. CT has an overall sensitivity of 96%, specificity of 98%, and accuracy of 97% [14]. CT findings consistent with hollow viscus and mesenteric injuries after blunt abdominal trauma include free fluid, extraluminal air, bowel wall thickening/discontinuity, mesenteric hematoma/streaking, and extravasation of oral contrast [15, 16]. In blunt abdominal trauma CT has a sensitivity of 94% for detecting bowel injury and 96% for identifying mesenteric injuries [17]. CT is time consuming, expensive, has limited applicability in hemodynamically unstable patients, and with the addition of contrast can increase the risk of allergic reactions and aspiration.
Ultrasound scans can detect as little as 100 mL of fluid in the peritoneal cavity, and thus are useful in detecting the presence of intraperitoneal hemorrhage/fluid. FAST has an overall sensitivity of 76-100% and specificity of 96-100% [18, 19]. Compared to other diagnostic studies employed in trauma, such as DPL and CT, advantages of utilizing ultrasonography include its safety, rapid results, lower costs, performance at the bedside especially in hemodynamically unstable patients, and its noninvasive nature [20]. Unstable patients with evidence of intraabdominal hemorrhage/fluid can be taken directly to the operating room without delay. Although the sensitivity of FAST for the detection of free intraperitoneal fluid remains high, only 40-50% of bowel injuries are typically identified [21]. Ultrasound scans are less sensitive for hollow viscus and organ specific injuries, operator dependent (accuracy improves with experience), and projects decreased image quality in obese patients.
In an effort to conserve resources while maximizing patient safety we have employed a combined diagnostic modality utilizing FAST and CT of the abdomen and pelvis in virtually all blunt abdominal trauma patients, including those with a seatbelt mark sign. FAST has been shown to be less sensitive for the detection of gastrointestinal tract injuries, and a seatbelt sign alone increases the incidence of hollow viscus injury by as much as 10% [22, 23]. With evidence that the presence of a seatbelt mark sign increases the incidence of hollow viscus injuries we felt compelled to retrospectively investigate our own blunt abdominal trauma patient population with a seatbelt sign.
In our series of 69 patients we have a total of 11 true positive, 54 true negative, and 4 false negative results. None of FAST exams performed in our study were interpreted as indeterminate. Patients with an indeterminate FAST are admitted for observation, serial abdominal examinations, and repeat FAST or completion of a CT or DPL.
Instead of performing an abdominal and pelvic CT scan in all patients with a negative FAST exam we chose to follow them clinically as outlined in our algorithm. Other than two deaths, the remaining 67 patients were all eventually discharged from the hospital. While the FAST exam was falsely negative in four patients, there were no missed injuries utilizing a combined modality of an initial ultrasound scan reinforced by CT. The sensitivity for utilizing FAST for detecting a clinically significant injury in this study is 73% with 100% specificity, a negative predictive value of 93%, positive predictive value of 100%, and accuracy of 94%.
With an initial negative FAST our algorithm calls for repeating an ultrasound scan with a change in the patient’s examination (drop in hemoglobin, abdominal pain, nausea and emesis, etc.). Unfortunately these are carried out at the bedside (outside of the trauma bay) and results are infrequently recorded, limiting our ability to adequately evaluate and discuss further in this paper. The applicability of our study to the neurologically impaired patient population is hindered since 90% of our series presented with a GCS of 15. Other limitations to this study include its retrospective nature, a single institution experience, and small patient population.
Conclusion
In conclusion the use of FAST, not as a single diagnostic modality, but as a screening tool with selective use of CT, is a relatively reliable instrument for the initial evaluation of the blunt abdominal trauma patient with a seatbelt mark sign.
Financial Disclosure
No financial support was received.
Abbreviations
FAST: focused assessment with sonography for trauma; GCS: Glasgow coma scale; CT: computerized tomography; DPL: diagnostic peritoneal lavage; IRB: Institutional Review Board
| References | ▴Top |
- Shults RA, Nichols JL, Dinh-Zarr TB, Sleet DA, Elder RW. Effectiveness of primary enforcement safety belt laws and enhanced enforcement of safety belt laws: a summary of the Guide to Community Preventive Services systematic reviews. J Safety Res. 2004;35(2):189-196.
doi pubmed - Denis R, Allard M, Atlas H, Farkouh E. Changing trends with abdominal injury in seatbelt wearers. J Trauma. 1983;23(11):1007-1008.
doi pubmed - Appleby JP, Nagy AG. Abdominal injuries associated with the use of seatbelts. Am J Surg. 1989;157(5):457-458.
doi - Asbun HJ, Irani H, Roe EJ, Bloch JH. Intra-abdominal seatbelt injury. J Trauma. 1990;30(2):189-193.
doi pubmed - Chandler CF, Lane JS, Waxman KS. Seatbelt sign following blunt trauma is associated with increased incidence of abdominal injury. Am Surg. 1997;63(10):885-888.
pubmed - Velmahos GC, Tatevossian R, Demetriades D. The "seat belt mark" sign: a call for increased vigilance among physicians treating victims of motor vehicle accidents. Am Surg. 1999;65(2):181-185.
pubmed - Garrett JW, Braunstein PW. The seat belt syndrome. J Trauma. 1962;2:220-238.
doi - Stassen NA, Lukan JK, Carrillo EH, Spain DA, Richardson JD. Abdominal seat belt marks in the era of focused abdominal sonography for trauma. Arch Surg. 2002;137(6):718-722; discussion 722-713.
- Miller MT, Pasquale MD, Bromberg WJ, Wasser TE, Cox J. Not so FAST. J Trauma. 2003;54(1):52-59; discussion 59-60.
doi pubmed - Fischer RP, Beverlin BC, Engrav LH, Benjamin CI, Perry JF, Jr. Diagnostic peritoneal lavage: fourteen years and 2,586 patients later. Am J Surg. 1978;136(6):701-704.
doi - Sato T, Hirose Y, Saito H, Yamamoto M, Katayanagi N, Otani T, Kuwabara S, et al. Diagnostic peritoneal lavage for diagnosing blunt hollow visceral injury: the accuracy of two different criteria and their combination. Surg Today. 2005;35(11):935-939.
doi pubmed - Jaffin JH, Ochsner MG, Cole FJ, Rozycki GS, Kass M, Champion HR. Alkaline phosphatase levels in diagnostic peritoneal lavage fluid as a predictor of hollow visceral injury. J Trauma. 1993;34(6):829-833.
doi pubmed - Meyer DM, Thal ER, Weigelt JA, Redman HC. Evaluation of computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma. 1989;29(8):1168-1170; discussion 1170-1162.
- Kearney PA, Jr., Vahey T, Burney RE, Glazer G. Computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. Their combined role. Arch Surg. 1989;124(3):344-347.
doi pubmed - Breen DJ, Janzen DL, Zwirewich CV, Nagy AG. Blunt bowel and mesenteric injury: diagnostic performance of CT signs. J Comput Assist Tomogr. 1997;21(5):706-712.
doi pubmed - Scaglione M, de Lutio di Castelguidone E, Scialpi M, Merola S, Diettrich AI, Lombardo P, Romano L, et al. Blunt trauma to the gastrointestinal tract and mesentery: is there a role for helical CT in the decision-making process? Eur J Radiol. 2004;50(1):67-73.
doi pubmed - Killeen KL, Shanmuganathan K, Poletti PA, Cooper C, Mirvis SE. Helical computed tomography of bowel and mesenteric injuries. J Trauma. 2001;51(1):26-36.
doi pubmed - Lee BC, Ormsby EL, McGahan JP, Melendres GM, Richards JR. The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. AJR Am J Roentgenol. 2007;188(2):415-421.
doi pubmed - Rozycki GS, Ballard RB, Feliciano DV, Schmidt JA, Pennington SD. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg. 1998;228(4):557-567.
doi pubmed - Boulanger BR, McLellan BA, Brenneman FD, Ochoa J, Kirkpatrick AW. Prospective evidence of the superiority of a sonography-based algorithm in the assessment of blunt abdominal injury. J Trauma. 1999;47(4):632-637.
doi pubmed - Richards JR, McGahan JP, Simpson JL, Tabar P. Bowel and mesenteric injury: evaluation with emergency abdominal US. Radiology. 1999;211(2):399-403.
doi pubmed - Yoshii H, Sato M, Yamamoto S, Motegi M, Okusawa S, Kitano M, Nagashima A, et al. Usefulness and limitations of ultrasonography in the initial evaluation of blunt abdominal trauma. J Trauma. 1998;45(1):45-50; discussion 50-41.
- Allen GS, Moore FA, Cox CS, Jr., Wilson JT, Cohn JM, Duke JH. Hollow visceral injury and blunt trauma. J Trauma. 1998;45(1):69-75; discussion 75-68.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
