| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Original Article
Volume 4, Number 3, September 2014, pages 91-94
Influence of Postoperative Bladder Washout on the Heart Rate: Cohort Study
Radwan Kassira, e, Leonard Feassonb, Vincent Pichotc, Paul Vercherind, Jean Claude Barthelemyc
aDepartment of General Surgery, CHU Hospital, Jean Monnet University, Saint Etienne, France
bExercise Physiology Laboratory, CHU Hospital, Jean Monnet University, Saint Etienne, France
cLaboratory of Autonomic Nervous System Activity, EA 407, CHU Hospital, Jean Monnet University, Saint Etienne, France
dDepartment of Public Health, CHU Hospital, Jean Monnet University, Saint Etienne, France
eCorresponding Author: Radwan Kassir, Department of General Surgery, CHU Hospital, Jean Monnet University, Avenue Albert Raimond, 42270 Saint Etienne, France
Manuscript accepted for publication April 14, 2014
Short title: Influence of Bladder Washout on Heart Rate
doi: https://doi.org/10.14740/jcs228w
| Abstract | ▴Top |
Background: Endoscopic urological surgery is a marginal invasive tool. However, sympathetic activity could be created during the postoperative sequences due to a bladder washout by means of a dynamic bladder filling.
Methods: We studied (cohort study) the preoperative and postoperative response of a patient’s heart rate during the dynamic bladder washout using Holter’s monitor.
Results: A total of 15 consecutive male patients aged from 65 to 96 years were included. There was a significant difference in the average heart rate (with P = 0.0053) (69.61 ± 8.83) before and (73.58 ± 11.14) during the process. There was no significant difference in the average low frequency (LF) (P = 0.217706) (349.30 ± 446.08) before and (304.54 ± 356.53) during the washout. There was no significant difference in the average high frequency (HF) (parasympathetic activity) (P = 0.116) (323.77 ± 471.92) before and (273.69 ±413.19) during the washout. The average before the LF/HF washout is 2.97 ± 3.50 and the average during the LF/HF washout is 3.91 ± 4.16. It showed limited significance (P = 0.054).
Discussion: The only significant result is that the bladder washout increases the heart rate by boosting the orthosympathetic activity. It is being studied that the sensation of the bladder filling is transmitted via the sympathetic hypogastric nerve (orthosympathetic activity). Nevertheless, it might be necessary to take a larger population sample with more homogeneous inclusion criteria.
Conclusion: We conclude that the postoperative bladder washout after transurethral resection of the prostate and bladder cancer significantly increases the heart rate.
Keywords: Bladder; Cardiology; Heart rate; Endoscopic urological; Autonomic nerve system; Cardiovascular risk factors
| Introduction | ▴Top |
The gradual filling of the bladder determines an increased sympathetic activity that is occurring quickly, and that is clinically felt once the filling reaches 40% of the bladder volume. The urination urge is imperious when 90% of the filling is at achieved. At the time of urination, the parasympathetic activity becomes critical, opens the detrusor muscle and contracts the bladder, thus withdrawing the sympathetic activity. In the postoperative context of the endoscopic prostate surgery, the post-surgical bladder filling is used to ensure the removal of intravesical clots. A question concerning the impact of a constant dynamic bladder filling maintenance arises since an increase of the sympathetic activity may have cardiovascular consequences. It is the same in certain cases of bladder endoscopic surgeries, where the same procedure of postoperative dynamic bladder filling is used. To answer this question, we propose a prospective longitudinal cohort study by measuring the sympathetic activity during the therapeutic dynamic bladder filling. To conduct this evaluation, we chose the heart rate as an index of the autonomic nervous system.
| Materials and Methods | ▴Top |
Patients
Inclusion criteria are male patients aged from 65 to 96 years hospitalized for transurethral resection of the bladder (TURB) or transurethral resection of prostate (TURP). Exclusion criteria are patients under cardiac treatment (Cordarone, antiarrhythmic, etc.) and the presence of heart diseases. All patients have given their consent to the study. Holter ECG is very accurate (300 Hz). The same Holter monitor brand was used of the brand (Vista Recorder, Novacor, Rueil-Malmaison). The Holter was placed at 8 pm of the night before the surgery and removed at 6 am of the next day: pre-washout Holter. Another recording was done at 6 pm after the surgery until 6 am in the next morning: Holter during washout. The frequency and the ANS activity were analyzed by means of the RR of Holter recordings. Spectral analysis of RR variability via the Fourier equation shows characteristic peaks allowing the calculation of indicators representing the autonomic nervous system activity. The most commonly used indicators are high frequencies (HFs) characterizing parasympathetic activity, low frequencies (LFs) exemplifying orthosympathetic and parasympathetic activities, and the LF/HF ratio describing the sympathovagal balance. Average comparisons were made using paired t-tests.
Methods
TURB
The intervention is performed under general anesthesia and it consists of the ablation or the removal of a bladder lesion to practically analyze it microscopically. Just like any surgical intervention, a preoperative anesthesia consultation is necessary a few days before surgery. This procedure is performed through natural openings, without abdominal surgery. The surgeon inserts into the urethra a device called an endoscopic resector. The operation is performed under visual control. The endoscopic resector allows removing the lesion and coagulating different vessels that are likely to bleed. At the end of the intervention, a probe/catheter with continuous washout is inserted into the bladder. The bladder washout is stopped once the urine is clear, and the urinary catheter is removed according to the surgeon.
TURP
The endoscopic resection does not remove the entire prostate, but the central part that is responsible of the obstacle only. This intervention does not protect from the subsequent development of a possible prostate cancer. This procedure is performed through natural orifice, without abdominal surgery. The surgeon inserts into the urethra a device called an endoscopic resector. The operation is performed under visual control. The endoscopic resector is equipped with an electrical loop that can cut the adenoma into small pieces and coagulate the prostate vessels. These pieces are removed from the bladder and sent to the laboratory for analysis. At the end of the intervention, a continuous washing probe/catheter is inserted into the bladder. The bladder washout is stopped as soon as the urine is clear, and the urinary catheter is removed according to the surgeon.
The bladder washout
The bladder washout is a technique which consists of continuously passing a stream of liquid into the bladder. This continuous cleaning of the bladder after a bladder or prostate endoscopic resection (TURB/TURP) aims at avoiding the formation of blood clots in the bladder. The filling, due to the regulation of the bladder inflow and outflow, determines a filling level of about 40% of the bladder volume. This level of filling should determine an increase in the sympathetic activity.
Holter variability ECG/study
The study of the heart rate variability, called “RR interval variability” or “RR variability”, has made a significant growth over the past two decades, when its close links with the autonomic nervous system activity were highlighted. Largely, the parasympathetic activity may determine rapid changes in the RR variability due to the short half-life of acetylcholine, which may determine a deceleration, and therefore an extension of RR, different for each beat; however, the orthosympathetic activity will result in slower changes in RR, including shortening of these intervals, because of the longer half-life of noradrenaline. By extracting the RR intervals of the ECG by an electrocardiogram, each R wave is detected in order to calculate the length of time intervals between two successive R waves. The obtained input, expressed in seconds or milliseconds, represents the sequence of RR intervals which reflects the opposite of the instantaneous heart rate of the person. These RR intervals are analyzed by Fourier equation which can identify HFs and LFs. The peak of LF is the result of orthosympathetic and parasympathetic activities, but its increase is usually interpreted as an increase in the orthosympathetic activity. The use and interpretation of this peak should not be done solely, but taking into account other indicators such as LFNU (LF power in normalized units) and the LF/HF ratio (Fig. 1).
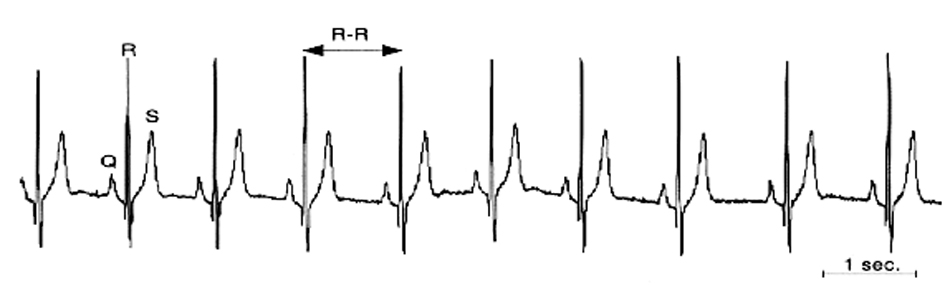 Click for large image | Figure 1. Extraction of sinusoidal RR intervals from ECG signals. |
This frequency band (HF) is typically considered to be related to the parasympathetic activity. Values of LF/HF ratio greater than 1 indicate orthosympathetic predominance and values less than 1 indicate parasympathetic predominance (Fig. 2).
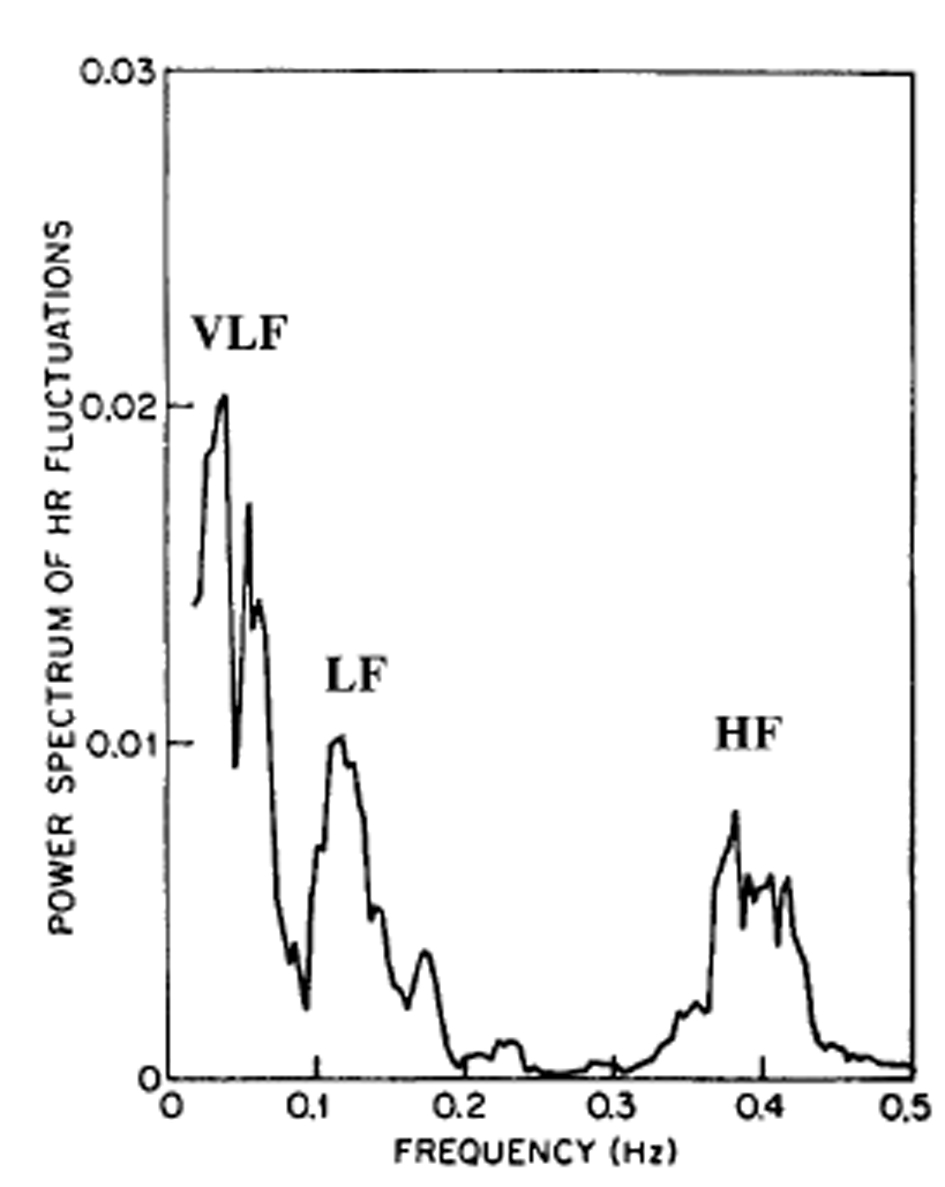 Click for large image | Figure 2. Fourier transform. |
| Results | ▴Top |
Fifteen consecutive male persons aged from 65 to 96 years were included (people involved in this type of surgery). There was a significant difference in the average heart rate (with P = 0.0053) (69.61 ± 8.83) before and during the process (73.58 ± 11.14). There was no significance in the average LF (P = 0.217706) (349.30 ±446.08) before and during the washout (304.54 ± 356.53). There was no significance in the average HF (parasympathetic activity) (P = 0.116) (323.77 ± 471.92) before and during the washout (273.69 ± 413.19). The average LF/HF before the washout is 2.97 ± 3.50 and the average LF/HF during the washout is 3.91 ± 4.16. It showed limited significance (P = 0.054).
| Discussion | ▴Top |
The sensitivities of the bladder and the sphincter system are decisive to the voluntary control of the urethral function [1]. For an adequate sensation, a normal urothelium lining, peripheral nervous system, spinal cord, brainstem, midbrain and sensory cortex is essential. A study of bladder filling sensations was conducted for the first time in the 1930s. This early knowledge has been confirmed by studies performed by Wyndaele [2, 3] in the 1990s, allowing the study of the normal functioning of the bladder sensation among healthy persons. It has been demonstrated that no urge sensation was perceived to an empty bladder after urination. As the bladder is being filled, the person’s sensation of filling appears as of nearly 40% of bladder capacity is reached (B2 urodynamic) [4, 5]. It is being studied that the sensation of bladder filling is transmitted via the sympathetic hypogastric nerve. After perception of about 60% of the maximum bladder filling capacity, the need for urination (B2 urodynamic) arises. If the bladder filling approaches its maximum, the sensation of urinary urge becomes greater and cannot be ignored for a longer time. When 90% of the bladder capacity is reached, a compelling need emerges (B3 urodynamic) described as constant and unpleasant perception in the urethral and perineal region [4, 5]. By mean of a voluntary contraction of the perineum it is still possible to inhibit the sensation and delay urination for a certain period of time. If the filling is not interrupted despite this sense of significant urinary urge, pain appears as can be seen in acute painful retention of urine.
The only significant result is that the bladder washout increases the heart rate by boosting the orthosympathetic activity. On the day of surgery, patients were operated under general anesthesia. The anesthesiologist injected different products depending on the age and weight of the patient; however, neither the age nor the weight is identical among patients. So each patient had a different dose of these molecules, keeping in mind that these molecules are not removed before a week of time. So we have here a perplexity. Nevertheless, it might be necessary to take a larger population sample with more homogeneous inclusion criteria. Little pain is present after the operation. Irritation is sometimes described and may contribute in the HR increase.
Conclusion
The bladder washout increases heart rate by increasing the orthosympathetic activity. This may represent an increased cardiovascular risk.
Conflict of Interests
No conflict of interests.
| References | ▴Top |
- Nathan PW. Sensations associated with micturition. Br J Urol. 1956;28(2):126-131.
doi pubmed - Denny-Brown D, Robertson EG. 'An investigation of the nervous control of defecation' by Denny-Brown and Robertson: a classic paper revisited. 1935. Colorectal Dis. 2004;6(5):376-383.
doi pubmed - Wyndaele JJ. Is impaired perception of bladder filling during cystometry a sign of neuropathy? Br J Urol. 1993;71(3):270-273.
doi pubmed - Wyndaele JJ. The normal pattern of perception of bladder filling during cystometry studied in 38 young healthy volunteers. J Urol. 1998;160(2):479-481.
doi - Wyndaele JJ, De Wachter S. Cystometrical sensory data from a normal population: comparison of two groups of young healthy volunteers examined with 5 years interval. Eur Urol. 2002;42(1):34-38.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
