| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website http://www.currentsurgery.org |
Original Article
Volume 4, Number 3, September 2014, pages 61-69
The Effect of Gender, Age and BMI on Postoperative C-Reactive Protein Levels After Major Abdominal Surgery
Jennifer Straatmana, c, Annelieke M.K. Harmsena, Miguel A. Cuestaa, Elly S.M. de Langeb, Donald L. van der Peeta
aDepartment of Gastrointestinal Surgery, VU Medical Center, Amsterdam, The Netherlands
bDepartment of Epidemiology and Biostatistics, VU Medical Center, Amsterdam, The Netherlands
cCorresponding Author: Jennifer Straatman, Department of Gastrointestinal Surgery, Vrije Universiteit Medical Center, De Boelelaan 1117, ZH 7F002, The Netherlands
Manuscript accepted for publication July 28, 2014
Short title: Factors on Postoperative CRP Levels
doi: https://doi.org/10.14740/jcs236w
| Abstract | ▴Top |
Background: The aim of this observational study was to analyze whether differences exist in postoperative C-reactive protein (CRP) levels in elderly, obese or for gender after major abdominal surgery, which might affect the diagnostic value of CRP.
Methods: Observational cohort study was made between January 2009 and January 2011 of all adult patients who underwent major abdominal surgery. Medical records and radiology were reviewed. Complications were recorded based on the classification by Clavien-Dindo. CRP data were collected up to 14 days postoperatively, or until discharge.
Results: Three hundred ninety-nine patients underwent major abdominal surgery. Seventy-four patients underwent upper gastrointestinal (GI) surgery, 91 patients underwent hepato-pancreatico-billiary (HPB) surgery and 234 underwent lower GI surgery. Two hundred thirty-five patients were male. Eighty-three patients presented with a major complication (20.8%). No effect of gender or age on postoperative CRP levels was observed. Although a positive correlation was observed for BMI, this did not hold in further regression analysis.
Conclusions: No effect was observed for gender, age and BMI on postoperative CRP levels. It is proposed that the effect of surgical trauma and inflammation surpasses the effect of these related patient factors. The results further support the use of CRP as an independent marker of postoperative inflammation and complications.
Keywords: C-reactive protein; Major abdominal surgery; Postoperative complications; Quality control; Patient characteristics
| Introduction | ▴Top |
Postoperative complications after major abdominal surgery are reported in up to 40% of patients and pose a major clinical problem due to their association with increased morbidity and mortality [1, 2]. Apart from increased morbidity and mortality rates it results in longer in-hospital stay, higher costs and even increased cancer recurrence rates [3, 4]. Early diagnosis and treatment are paramount to improve these outcomes [5-8].
It is of interest to find an early, sensitive and specific marker that identifies patients at risk of postoperative complications, since complications may only become clinically evident as late as 8 - 12 days postoperatively, when patients present with critical illness [9, 10].
In search for this early marker for complications the focus of interest has been on C-reactive protein (CRP). CRP is a well-established marker for inflammation since levels are determined only by their rate of synthesis, independent of diet, diurnal rhythm or organ function [11]. Several studies have assessed the use of CRP as a marker for anastomotic leakage [12-14] or septic complications [15-17]. The use of CRP has been researched in upper gastrointestinal (GI), hepatico-pancreatico-billiary (HPB) and colorectal resections with similar results [18-20].
The recommended reference range for serum CRP is usually not corrected for patient characteristics such as gender, age or BMI. The effect of gender, age and BMI on CRP levels after major abdominal surgery has yet to be determined. This is of interest since it is shown that obese people have a threefold higher baseline CRP than normal weight patients do [21]. Furthermore, baseline CRP levels have shown to increase with age, which might reflect increasing incidence of subclinical pathologies [22]. Studies with induced inflammation show a faster increase in CRP in women, compared to men [23]. One could theorize these subgroups to be cofounders for postoperative serum CRP levels when CRP levels differ between these subgroups, since serum CRP levels are not only influenced by the surgical stress and inflammation. This might affect the interpretation of postoperative CRP levels. We sought to determine what influence age, sex and BMI have on the distribution of postoperative CRP levels. Given the rise of obesity and ageing in the general population it is of interest to see if postoperative CRP levels are still usable in the same fashion for these patients. The aim of this observational study was to analyze the diagnostic value of CRP for the prediction of major postoperative complications in different patient categories.
| Materials and Methods | ▴Top |
Study design
Observational cohort study was made of all adults who underwent major abdominal surgery in the VU Medical Center, Amsterdam, between January 2009 and January 2011. Major abdominal surgery was defined as all major resections of the upper GI tract, HPB organs or lower GI tract with reconstruction with either primary anastomosis and/or ostomy.
Both laparoscopic and open procedures were included, and procedures for benign and malignant disease were included. Acute procedures were also included.
Baseline characteristics were recorded: age, gender, height, weight, BMI, morbidity, American Society of Anesthesiologists (ASA) classification, preoperative blood sampling; hemoglobin, leukocytes, creatinine and CRP, along with indication for operation, procedure, duration of surgery, perioperative blood loss, complications, hospital and intensive care admission and mortality.
BMI was defined as an individual’s body mass (kg) divided by the square of their height (m); normal weight persons have a BMI below 25 kg/m2 and overweight persons have a BMI above 25 kg/m2.
Common practice in the VU Medical Center is to measure the CRP once postoperatively; additional measurements of CRP levels were performed if the physician deemed it necessary. CRP data were collected up to 14 days postoperatively, or until discharge. CRP measurement was performed in peripheral blood samples with Roche Modular P800 chemistry analyzer.
Clinical deterioration and increase in CRP and/or leucocytes implicated additional examinations, generally consisting of an enhanced CT scan, to preclude complications. CT scans were performed in a Philips 256 slice Brilliance iCT scanner, with oral, rectal and intravenous contrast. All patients received perioperatively prophylactic intravenous antibiotics and thromboprophylaxis according to local protocol.
If a major complication was diagnosed, treatment was initiated immediately. Interventions consisted of relaparotomy, percutaneous drainage or intensive care admission.
All postoperative complications were recorded and based on the classification by Clavien-Dindo, which was modified into minor and major complications as seen in other recent articles [24, 25]; classified as either minor complications, which require medical treatment or opening of the wound at the bedside, consisting of grade I and II of the Clavien-Dindo classification; or major complications, which require invasive treatment such as surgery or percutaneous drainage and intensive monitoring and consist of grades III, IV and V of the Clavien-Dindo classification [26].
Statistical analysis
Continuous variables are presented as means and standard deviations (SD) as a central tendency for normal distributions or as medians and ranges, as central tendency for non-normal distributions. Comparison of both groups was conducted with t-test analysis. Categorical variables are expressed as percentage frequencies and compared with Chi-square analysis as appropriate. Continuous variables are correlated with according P-values and R-square. A value of P < 0.05 was considered statistically significant. After assessment of linearity a linear regression was performed to assess the effect of gender, age and BMI on postoperative serum CRP levels and correct for confounding.
| Results | ▴Top |
Between January 2009 and December 2010, 399 patients underwent major abdominal surgery. Seventy-four patients (18.5%) underwent upper GI surgery, another 91 patients underwent HPB surgery (22.8%) and a final 234 of them underwent lower GI surgery (58.6%). Baseline characteristics are depicted in Table 1. Two hundred thirty-five out of 399 patients were male (58.9%).
 Click to view | Table 1. Baseline Characteristics |
Eighty-three patients presented with a major complication (20.8%), requiring a reoperation in 52 of them. Percutaneous drainage was performed in another 17 patients. Another nine patients were admitted to an intensive care unit for extra support and monitoring. Five patients died without reintervention (one due to postoperative bleed, one due to fulminant sepsis and three due to respiratory insufficiency caused by a respiratory infection).
CRP
In 18 patients no CRP data were available, and these patients were excluded for further CRP analysis. No statistically significant differences were observed in postoperative CRP levels in the three different organ groups. For instance, on postoperative day 3, average CRP was 189 mg/L in upper GI, 175 mg/L in HPB and 199 mg/L in lower GI surgery (P = 0.406).
Gender
Of all patients 58.9% were male. Average CRP levels showed no statistically significant differences between male and female patients with Student’s t-test. Further analysis of differences in gender in the uncomplicated/minor complicated group compared to the group of patients with major complications with Student’s t-test and appropriate Bonferroni correction again showed no statistically significant differences for gender. Figure 1 depicts average CRP levels for these groups with corresponding P-values.
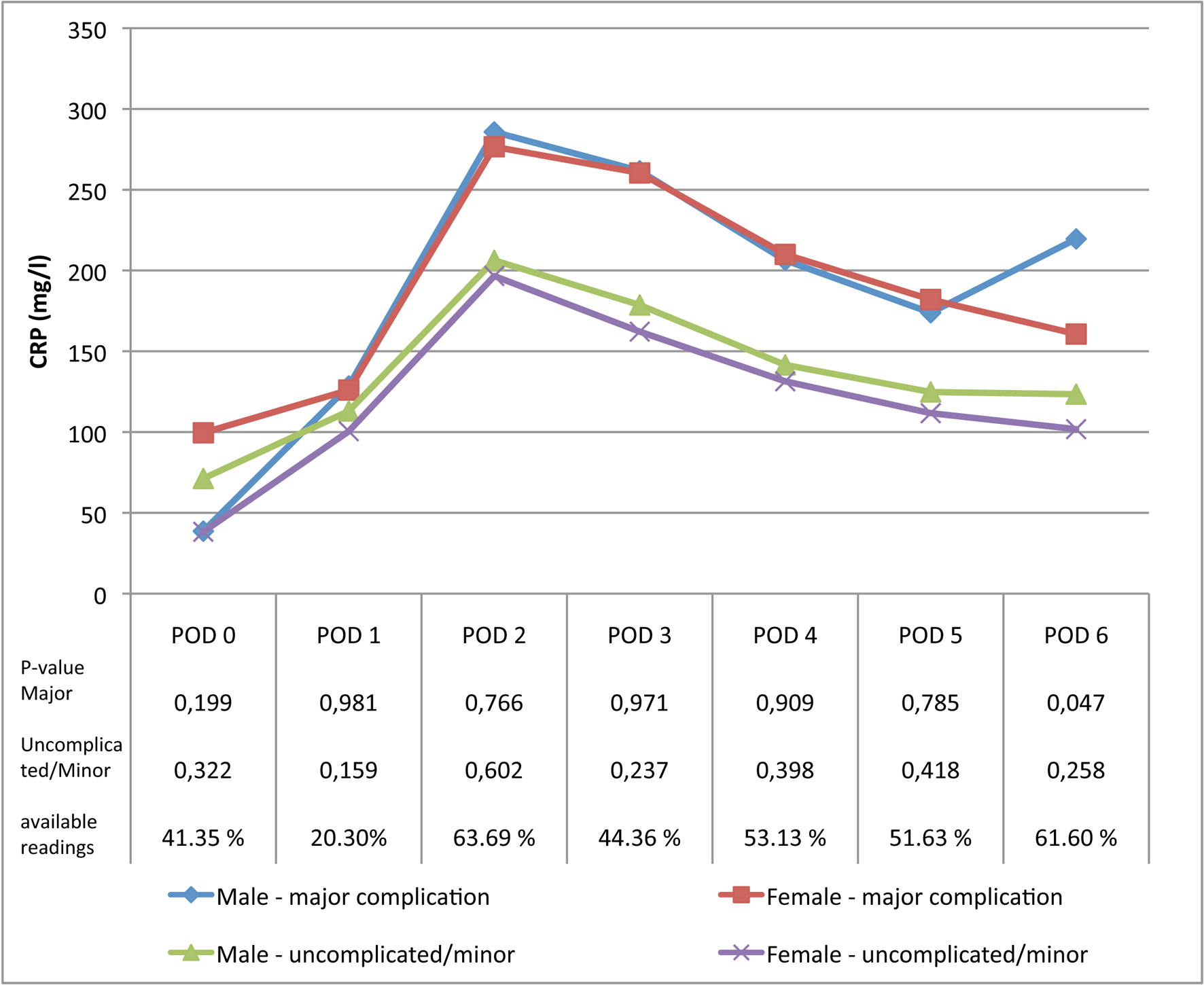 Click for large image | Figure 1. Average CRP levels in male and female patients with a minor or uncomplicated postoperative course and male and female patients with major complications. |
Age
Mean age was 60.2 years (SD 15.5 years). Using a Spearman’s correlation technique, no significant correlation was seen between age and CRP levels. Furthermore, separate analysis of patients with a major complication again did not show any statistically significant correlation, as depicted in Table 2. Furthermore, we divided patients into two groups, based on the statutory Dutch retirement age of 65 years at the time of inclusion. No statistically significant differences were observed in CRP values between patients younger or older than 65 years of age, even with further analysis within two complication groups (uncomplicated and minor complications versus major complications) as depicted in Figure 2.
 Click to view | Table 2. Correlation Between CRP Levels and Age in the Overall Group and Within the Group of Patients With Major Complications, Correlation Coefficients and P-Values Depicted |
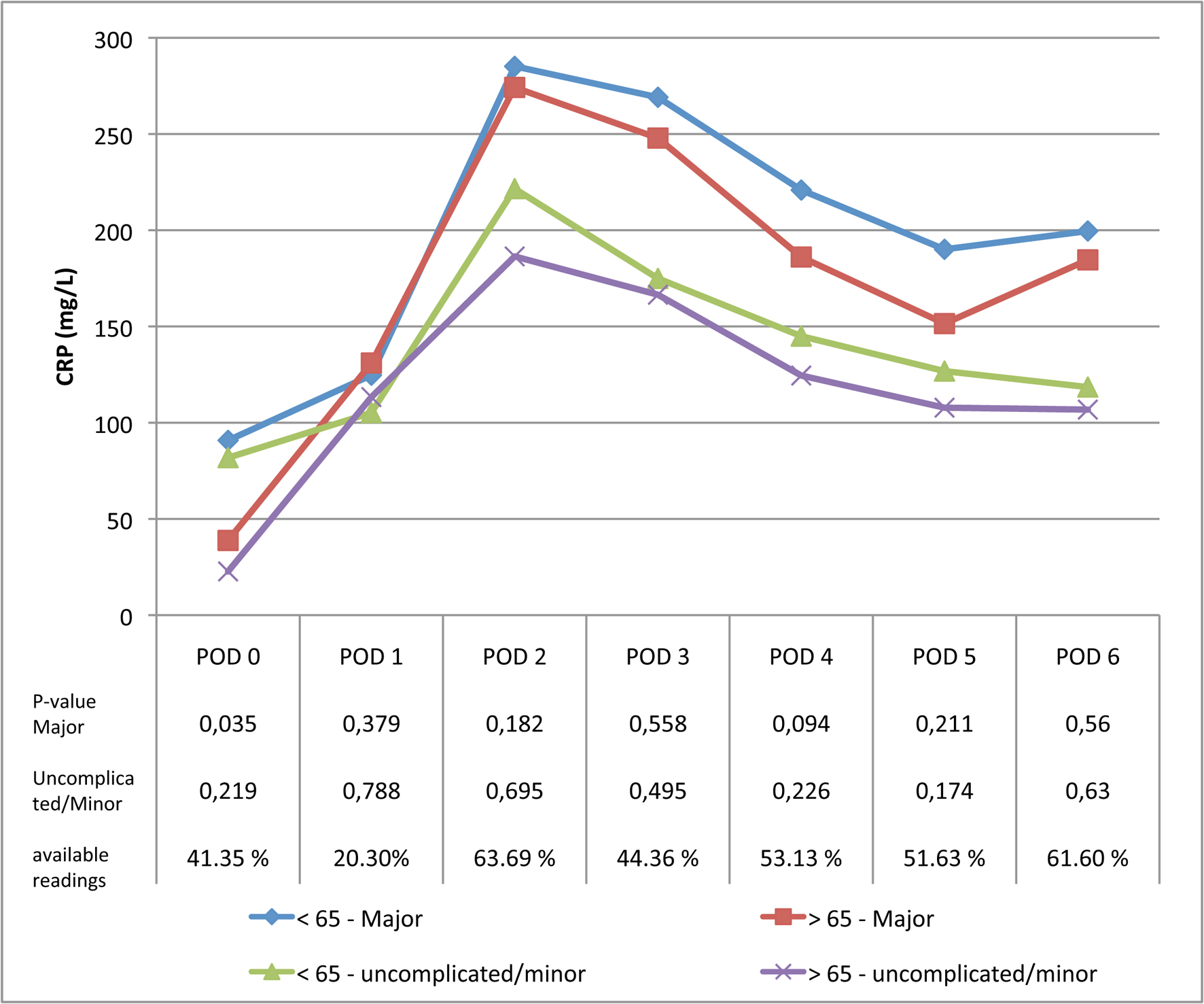 Click for large image | Figure 2. Average CRP levels in patients younger or older than 65 years with a minor or uncomplicated postoperative course and patients younger or older than 65 years with major complications. |
BMI
Mean BMI was 25.1 kg/m2 (SD 5.3 kg/m2). Using the Spearman’s correlation technique we found BMI to correlate with CRP levels on POD 0 - 4, with a maximum correlation of 0.280 on POD 0 (Table 3). Based on the limit of a BMI of 25 kg/m2, to differentiate between overweight and normal weight patients, patients were divided into two groups. Here, no statistically significant differences were observed, as portrayed in Figure 3.
 Click to view | Table 3. Correlation Between CRP Levels and BMI in the Overall Group and Within the Group of Patients With Major Complications, Correlation Coefficients and P-Values Depicted |
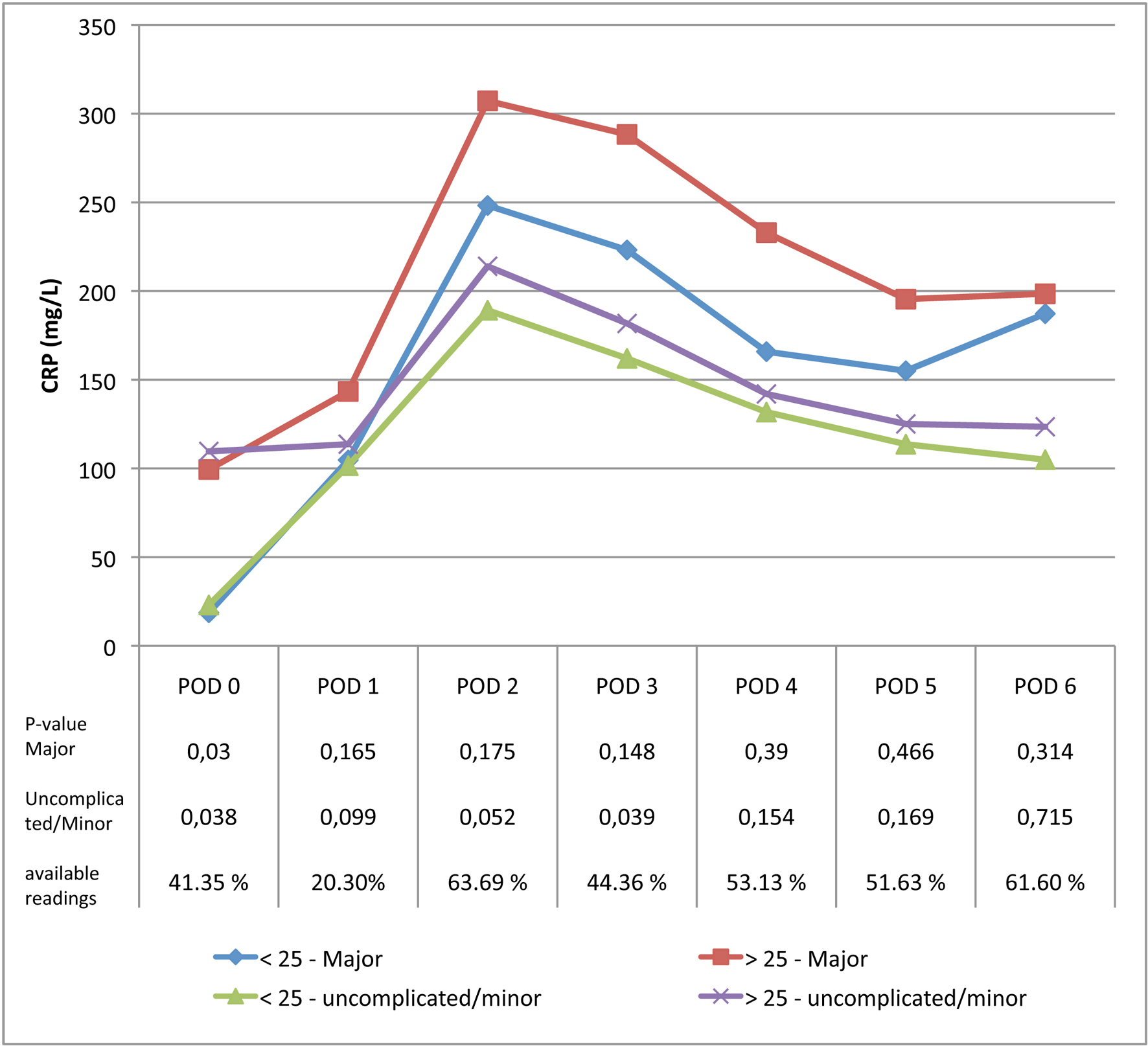 Click for large image | Figure 3. Average CRP levels in patients with a BMI above or below 25 kg/m2 with a minor or uncomplicated postoperative course and patients with a BMI above or below 25 kg/m2 with major complications. |
In order to further analyze the effect of the correlation between BMI and CRP on a cut-off as a predictor of complications, a linear regression analysis was conducted on postoperative days 3, 4 and 5. Coefficients are depicted in Table 4. R-square was 0.027 or lower. When regarding the two BMI groups in the regression analysis, no statistically significant effect was observed (P = 0.172).
 Click to view | Table 4. Linear Regression Coefficients for BMI and CRP Levels on Postoperative Days 3, 4 and 5 |
| Discussion | ▴Top |
Aim of the study presented here was to determine the effect of patient characteristics such as gender, age and BMI on postoperative CRP levels. No statistically significant effect was found for age and gender. For BMI a positive correlation was found; however, with regression techniques the R-square was 0.027 or lower, implying a negligible effect of BMI on postoperative CRP levels.
An analysis of CRP levels in a general adult population, including 2,895 males and 2,853 females, showed CRP levels to be twice as high in patients aged 65 - 74 years compared to patients aged 25 - 35 years old, respectively, 2 mg/L compared to 1 mg/L. Moreover, CRP values tended to be higher in females [22]. This study was conducted in healthy non-hospitalized patients [21]. After administration of endotoxin, a more proinflammatory response is seen in women compared to men, with a higher rise in CRP levels [23], although a higher cut-off for CRP levels is observed for male patients with induced endotoxemia in another study [27]. The study presented here showed no statistically significant effect of gender and age on postoperative CRP levels. A theory could be that baseline CRP differs among our patient group as well, and this implies that the effect of surgical trauma and inflammation greatly surpasses the effect of patient factors [28].
In research considering markers for coronary heart disease baseline CRP levels are highly associated with BMI [29]. This is attributed to the fact that interleukin-6 (IL-6), which amongst others is produced by adipocytes, activates transcription factors in the liver in order to produce CRP [30]. In the series presented here a positive correlation was observed. Upon linear regression analysis a statistically significant effect was observed, with an R-square of 2.7% or less. Further analysis determined the increase in CRP in obese patients to be negligible. We therefore concluded BMI to affect baseline CRP levels, but no significant effect is observed after major abdominal surgery.
After colorectal resection a peak in CRP levels is observed 48 - 96 h after surgery. In patients with an uncomplicated postoperative course CRP levels decrease after this peak [31]. When the inflammatory stimulus decreases, CRP levels decrease and finally return to baseline levels. Based on the data presented here we propose that this peak stimulus of surgical trauma and inflammation is the major determinant of postoperative CRP levels and are not significantly influenced by gender, age and BMI. These findings further support the use of CRP as a marker for postoperative complications and imply that established cut-offs for CRP do not need to be adjusted for age, gender or BMI. Along with earlier findings that CRP levels are not influenced by diet, circadian rhythm or organ function, this further establishes CRP as an independent marker of inflammation after major abdominal surgery.
Our study has several limitations. For one data were pooled for patients from different surgical sites, upper GI tract, HPB and lower GI-tract, though no statistically significant differences were observed between the three groups. Moreover, preliminary data show that pooling of data on laparoscopic and open procedures as well as benign and malignant and acute versus elective procedures showed no significant differences. The main limitation of this study is its observational nature. CRP measurements were only performed once as a single postoperative control and additionally when indicated by the attending physician. This could reflect the lack of data in the absence of any clinical symptoms prompting such a measurement.
To our knowledge the study presented here is the first that researched the effect of gender, age and BMI on postoperative CRP levels. No effect of gender or age was observed. Although a positive correlation was observed for BMI, this did not hold in further regression analysis. It is proposed that the effect of surgical trauma and inflammation surpasses the effect of patient factors such as gender, age and BMI. These results further support the use of CRP as an independent marker of postoperative inflammation and complications.
Funding
No funding was received.
Conflict of Interest
The authors declare no conflicts of interest.
| References | ▴Top |
- Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg. 2005;140(3):278-283, discussion 284.
doi pubmed - Velasco E, Thuler LC, Martins CA, Dias LM, Conalves VM. Risk factors for infectious complications after abdominal surgery for malignant disease. Am J Infect Control. 1996;24(1):1-6.
doi - Alves A, Panis Y, Pocard M, Regimbeau JM, Valleur P. Management of anastomotic leakage after nondiverted large bowel resection. J Am Coll Surg. 1999;189(6):554-559.
doi - Miccini M, Borghese O, Scarpini M, Cassini D, Gregori M, Amore Bonapasta S, Tocchi A. Anastomotic leakage and septic complications: impact on local recurrence in surgery of low rectal cancer. Ann Ital Chir. 2011;82(2):117-123.
pubmed - Rivers EP, Coba V, Whitmill M. Early goal-directed therapy in severe sepsis and septic shock: a contemporary review of the literature. Curr Opin Anaesthesiol. 2008;21(2):128-140.
doi pubmed - Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368-1377.
doi pubmed - Puskarich MA, Marchick MR, Kline JA, Steuerwald MT, Jones AE. One year mortality of patients treated with an emergency department based early goal directed therapy protocol for severe sepsis and septic shock: a before and after study. Crit Care. 2009;13(5):R167.
doi pubmed - Warschkow R, Beutner U, Steffen T, Muller SA, Schmied BM, Guller U, Tarantino I. Safe and early discharge after colorectal surgery due to C-reactive protein: a diagnostic meta-analysis of 1832 patients. Ann Surg. 2012;256(2):245-250.
doi pubmed - Buchs NC, Gervaz P, Secic M, Bucher P, Mugnier-Konrad B, Morel P. Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis. 2008;23(3):265-270.
doi pubmed - Petersen S, Freitag M, Hellmich G, Ludwig K. Anastomotic leakage: impact on local recurrence and survival in surgery of colorectal cancer. Int J Colorectal Dis. 1998;13(4):160-163.
doi pubmed - Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111(12):1805-1812.
doi - Ortega-Deballon P, Radais F, Facy O, d'Athis P, Masson D, Charles PE, Cheynel N, et al. C-reactive protein is an early predictor of septic complications after elective colorectal surgery. World J Surg. 2010;34(4):808-814.
doi pubmed - Korner H, Nielsen HJ, Soreide JA, Nedrebo BS, Soreide K, Knapp JC. Diagnostic accuracy of C-reactive protein for intraabdominal infections after colorectal resections. J Gastrointest Surg. 2009;13(9):1599-1606.
doi pubmed - Guirao X, Juvany M, Franch G, Navines J, Amador S, Badia JM. Value of C-reactive protein in the assessment of organ-space surgical site infections after elective open and laparoscopic colorectal surgery. Surg Infect (Larchmt). 2013;14(2):209-215.
doi pubmed - Warschkow R, Tarantino I, Torzewski M, Naf F, Lange J, Steffen T. Diagnostic accuracy of C-reactive protein and white blood cell counts in the early detection of inflammatory complications after open resection of colorectal cancer: a retrospective study of 1,187 patients. Int J Colorectal Dis. 2011;26(11):1405-1413.
doi pubmed - Platt JJ, Ramanathan ML, Crosbie RA, Anderson JH, McKee RF, Horgan PG, McMillan DC. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19(13):4168-4177.
doi pubmed - Welsch T, Muller SA, Ulrich A, Kischlat A, Hinz U, Kienle P, Buchler MW, et al. C-reactive protein as early predictor for infectious postoperative complications in rectal surgery. Int J Colorectal Dis. 2007;22(12):1499-1507.
doi pubmed - Welsch T, Frommhold K, Hinz U, Weigand MA, Kleeff J, Friess H, Buchler MW, et al. Persisting elevation of C-reactive protein after pancreatic resections can indicate developing inflammatory complications. Surgery. 2008;143(1):20-28.
doi pubmed - MacKay GJ, Molloy RG, O'Dwyer PJ. C-reactive protein as a predictor of postoperative infective complications following elective colorectal resection. Colorectal Dis. 2011;13(5):583-587.
doi pubmed - Warschkow R, Tarantino I, Ukegjini K, Beutner U, Muller SA, Schmied BM, Steffen T. Diagnostic study and meta-analysis of C-reactive protein as a predictor of postoperative inflammatory complications after gastroesophageal cancer surgery. Langenbecks Arch Surg. 2012;397(5):727-736.
doi pubmed - Wener MH, Daum PR, McQuillan GM. The influence of age, sex, and race on the upper reference limit of serum C-reactive protein concentration. J Rheumatol. 2000;27(10):2351-2359.
pubmed - Hutchinson WL, Koenig W, Frohlich M, Sund M, Lowe GD, Pepys MB. Immunoradiometric assay of circulating C-reactive protein: age-related values in the adult general population. Clin Chem. 2000;46(7):934-938.
pubmed - van Eijk LT, Dorresteijn MJ, Smits P, van der Hoeven JG, Netea MG, Pickkers P. Gender differences in the innate immune response and vascular reactivity following the administration of endotoxin to human volunteers. Crit Care Med. 2007;35(6):1464-1469.
doi pubmed - Strong VE, Devaud N, Allen PJ, Gonen M, Brennan MF, Coit D. Laparoscopic versus open subtotal gastrectomy for adenocarcinoma: a case-control study. Ann Surg Oncol. 2009;16(6):1507-1513.
doi pubmed - Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187-196.
doi pubmed - Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205-213.
doi pubmed - Ferguson JF, Patel PN, Shah RY, Mulvey CK, Gadi R, Nijjar PS, Usman HM, et al. Race and gender variation in response te evoked inflammation. Journal of Translational Medicine. 2013;11(63):1-9.
- Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut. 2006;55(3):426-431.
doi pubmed - Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279(18):1477-1482.
doi pubmed - Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW. C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol. 1999;19(4):972-978.
doi pubmed - Kragsbjerg P, Holmberg H, Vikerfors T. Serum concentrations of interleukin-6, tumour necrosis factor-alpha, and C-reactive protein in patients undergoing major operations. Eur J Surg. 1995;161(1):17-22.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
