| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website https://www.currentsurgery.org |
Case Report
Volume 11, Number 1, March 2021, pages 21-23
A Rare Case of Anterior Chamber SF6 Gas as a Complication of Pneumatic Retinopexy
Emanuela Interlandia, Francesco Pellegrinib, Paul Nderituc, g, Lorenzo Mottad, Erika Mandarae, Daniele Cironef
aDepartment of Ophthalmology, “Ospedale del Mare”, Naples, Italy
bDepartment of Ophthalmology, “Santo Spirito” Hospital, Pescara, Italy
cDepartment of Ophthalmology, Kings College Hospital, London, UK
dDepartment of Ophthalmology, East Kent Hospitals University, Kent, UK
eDepartment of Ophthalmology, Maria Paterno Arezzo Hospital, Ragusa, Italy
fDepartment of Ophthalmology, Casa di cura Villa Anna ,San benedetto del Tronto, Italy
gCorresponding Author: Paul Nderitu, Department of Ophthalmology, Kings College Hospital, London, UK
Manuscript submitted January 14, 2021, accepted January 21, 2021, published online February 26, 2021
Short title: SF6 in the AC After Pneumatic Retinopexy
doi: https://doi.org/10.14740/jcs434
| Abstract | ▴Top |
Pneumatic retinopexy is a surgical option for the treatment of retinal detachment. Although it is a generally safe procedure, it can be associated with a number of complications. We report a case of a 52-year-old man with a history of penetrating keratoplasty for keratoconus who underwent sulfur hexafluoride pneumatic retinopexy for a left acute rhegmatogenous macula-on retinal detachment. During the procedure, the patient suffered from a rare complication, a gas bubble that completely filled the anterior chamber during a pressure releasing paracentesis. The complication was successfully managed by extracting the gas with a cannula technique. In this case report, we discuss the current literature, possible etiologies and an approach to successful management for this rare complication.
Keywords: Anterior chamber; Vitreoretinal; Pneumatic retinopexy; Sulfur hexafluoride; Rhegmatogenous retinal detachment
| Introduction | ▴Top |
Pneumatic retinopexy (PR) is a trans-conjunctival surgical procedure for the treatment of primary rhegmatogenous retinal detachment (RD). Prior studies report PR combined with trans-conjunctival cryotherapy has a 90% success rate for the treatment of rhegmatogenous RD at 6 months [1]. Although PR is a safe procedure, adverse events have been described in the literature. Potential complications attributed to PR include subconjunctival gas, treatment failure, multiple gas bubbles, delayed subretinal fluid absorption, new retinal breaks, subretinal gas injection, vitreous inflammation, endophthalmitis and gas in the previtreous space [2]. PR can be advantageous compared to scleral buckling and vitrectomy as the procedure is less invasive, has fewer significant complications and does not require hospital admission [2]. We report of a rare complication of gas in the anterior chamber (AC) during PR and demonstrate our successful management approach for this rare complication.
| Case Report | ▴Top |
A 52-year-old man was referred for the surgical treatment of an acute (1-day history) rhegmatogenous RD in the left eye. The patient underwent penetrating keratoplasty (PK) in the same eye 10 years previously for keratoconus. Best corrected visual acuity was 20/20 in the right eye and 20/40 OS. Slit lamp and fundal examination were unremarkable in the right eye. There was no an iridotomy in the left eye where the lens was transparent and stable. Fundus examination revealed a 2 o’clock retinal tear with a limited (3 clock hours) superotemporal RD with an attached macula and vitreous. PR was performed the following day. After cryopexy, a superior paracentesis was performed and 0.3 mL of aqueous drained from the AC. Undiluted sulfur hexafluoride (SF6) (0.5 mL) was injected via the pars plana infero-temporally. Upon examination, the central retinal artery was non-perfused; hence more AC aqueous was drained from the paracentesis. Upon performance of the AC draining, a gas bubble completely filled the AC (Fig. 1). The gas bubble was successfully managed by removal with a cannula (Figs. 2, 3) and the patient was given instructions on correct positioning. The retina was attached 3 days after procedure, but a new tear associated with vitreous hemorrhage developed after 1 month which was successfully managed with a vitrectomy without further adverse clinical events.
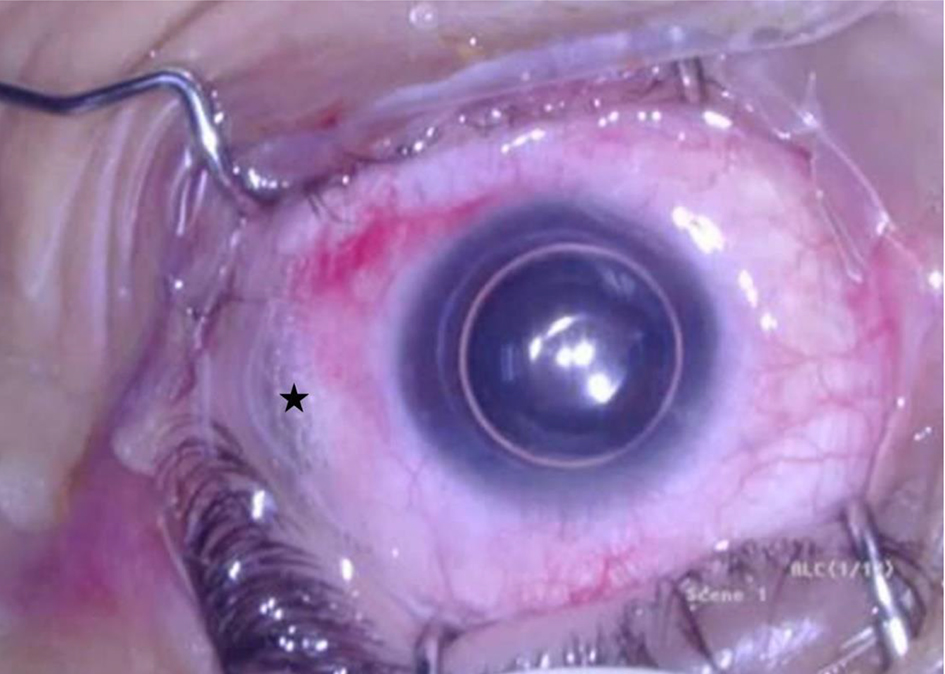 Click for large image | Figure 1. Gas filling the anterior chamber after the drainage of aqueous. Surgeon’s view, left eye. Note a small amount of subconjunctival gas in the site of injection (indicated by the black star). |
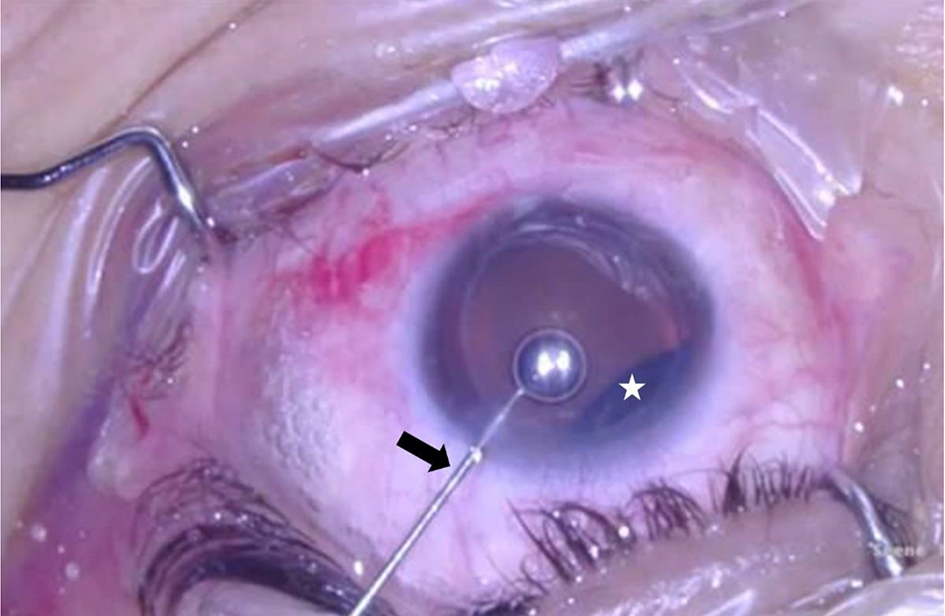 Click for large image | Figure 2. Extraction of gas using a cannula. Surgeon’s view, left eye. A cannula is introduced through the superotemporal paracentesis (indicated by the black arrow) and the gas is completely removed. Intravitreal gas evident superonasally (indicated by the white star). |
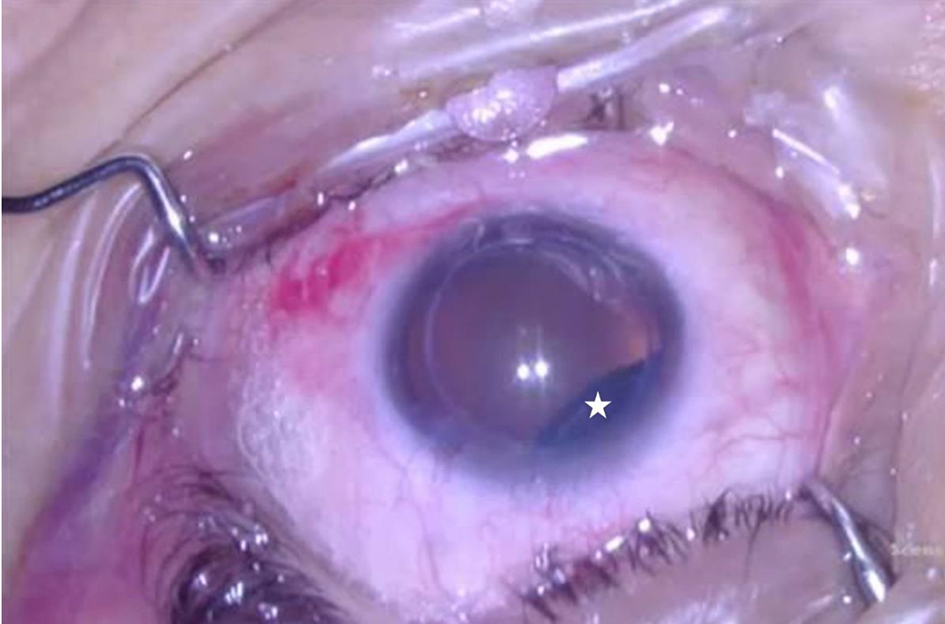 Click for large image | Figure 3. Post successful management of gas in the anterior chamber. Surgeon’s view, left eye. Intravitreal gas evident superonasally (indicated by white star). |
| Discussion | ▴Top |
PR is a relatively non-invasive and rapid procedure useful in the management of selected cases of rhegmatogenous RD. Since its introduction in 1986 [1], PR has become an alternative surgical technique to scleral buckling (SB) and pars plana vitrectomy (PPV) in uncomplicated RD with superior retinal breaks. The advantages of PR in comparison with SB and PPV are reduced invasiveness, surgical times, major complications, treatment costs and no requirement for hospital admission [2].
Although PR is a safe procedure, several complications including subconjunctival or subretinal gas, vitreous hemorrhage, new retinal breaks, treatment, proliferative vitreoretinopathy and delayed reabsorption of subretinal fluid have been described [3, 4]. Less frequent complications include endophthalmitis, macular folds, angle-closure glaucoma, macular hole, vitreous loss, iris and vitreous incarceration at the paracentesis, cystoid macular edema, macular pucker, choroidal detachment, myopic shift, ischemic optic neuropathy, retinal vascular occlusion and gas entrapment in pre-hyaloid space and/or in AC.
A literature search was undertaken to identify reports of PR complicated by AC gas. Electronic literature searches were performed using PubMed and Google Scholar. Search terms were “pneumatic retinopexy” AND “anterior chamber” AND “gas”. Following this search, the references of identified articles were further reviewed to identify additional relevant articles. Our search found a limited number of articles describing AC gas entrapment as a complication of PR, with only two reported cases in the current literature [5, 6]. Gas in the AC after PR is thought to be an extension of pre-hyaloidal gas entrapment. In 2001, Taher and Haimovici reported a case of migration of gas to the AC in a phakic eye after PR [5]. They hypothesized that the gas was injected in the virtual space between the lens and the anterior hyaloid (canal of Petit). The forceful injection of a relatively large volume (0.6 mL) of gas in this small space created a pressure gradient leading to a zonular dehiscence and consequent AC gas entrapment.
In 2011, Tan et al described a case of AC gas bubble of a young phakic patient who underwent PR [6]. However, they postulated that rather than zonular dehiscence, the loss of aqueous from the AC is the most likely precipitating factor by causing a sudden, large pressure gradient that favors anterior migration of the gas. The authors reached this conclusion because their patient was younger (45 vs. 62 years), so zonules should have been more resistant. Similarly, in their case, no significant zonular dehiscence or phacodonesis was noted after the migration of the gas bubble, a relatively small volume of gas was injected (0.3 vs. 0.6 mL) and finally migration of gas occurred only after paracentesis was performed.
Our patient is a phakic and relatively young man, in the absence of previous ocular trauma or iridotomy. The migration of the gas occurred after the second paracentesis and we did not observe zonular dehiscence or phacodonesis after anterior gas migration. In agreement with Tan and co-workers, we hypothesize that a gas bubble, regardless of its volume, where accidentally injected into the canal of Petit, can migrate anteriorly if there is the formation of a large pressure gradient. The sudden loss of aqueous immediately after a paracentesis and consequent pressure drop in AC pressure can create this large gradient.
PR is a useful surgical technique in selected cases of rhegmatogenous RD, but it is not complication-free. Vitreoretinal surgeons must keep in mind that anterior gas migration, although rare, is a potential complication of PR. Paracentesis, although beneficial, is a crucial moment in the procedure and should be gently performed when there is a gas bubble potentially trapped within the pre-hyaloid space.
Acknowledgments
We would like to thank the patient, whose clinical details are included in this case report, for their participation.
Financial Disclosure
The authors have no financial disclosure to declare.
Conflict of Interest
The authors declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Informed Consent
Written informed consent was obtained to publish the case report (including images).
Author Contributions
EI and FP collected the study data and images. EI, FP, PN, LM, EM and DC drafted the inital study manuscipt. PN and LM edited the draft manuscript and images. EI, FP, PN, LM, EM and DC reviewed and approved the final study manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Hilton GF, Grizzard WS. Pneumatic retinopexy. A two-step outpatient operation without conjunctival incision. Ophthalmology. 1986;93(5):626-641.
doi - Chan CK, Lin SG, Nuthi AS, Salib DM. Pneumatic retinopexy for the repair of retinal detachments: a comprehensive review (1986-2007). Surv Ophthalmol. 2008;53(5):443-478.
doi pubmed - Grizzard WS, Hilton GF, Hammer ME, Taren D, Brinton DA. Pneumatic retinopexy failures. Cause, prevention, timing, and management. Ophthalmology. 1995;102(6):929-936.
doi - Wirostko WJ, Han DP, Perkins SL. Complications of pneumatic retinopexy. Curr Opin Ophthalmol. 2000;11(3):195-200.
doi pubmed - Taher RM, Haimovici R. Anterior chamber gas entrapment after phakic pneumatic retinopexy. Retina. 2001;21(6):681-682.
doi pubmed - Tan C, Wee K, Zaw MD, Lim TH. Anterior chamber gas bubble following pneumatic retinopexy in a young, phakic patient. Clin Exp Ophthalmol. 2011;39(3):276-277.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
