| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website https://www.currentsurgery.org |
Original Article
Volume 14, Number 1, May 2024, pages 5-10
Colorectal Surgery Outcomes in Patients With Connective Tissue Disease: Insights From a National Database Analysis
Adejoke Johnsona, f , Ezekiel Akpana, Marianne Solanob, Medha Rajamanuric, Chukwunonso Ezeanid, Khan Zinobiae, Moses Bachane
aDepartment of Internal Medicine, Jacobi Medical Center/North Central Bronx Hospital, New York, NY, USA
bFaculty of Science and Health, University of Carabobo, Aragua, Naguanagua, Venezuela
cSouthern Illinois University, School of Medicine, Springfield, IL, USA
dBaton Rouge General Medical Center, Baton Rouge, LA, USA
eDepartment of Internal Medicine, James J. Peters VA Medical Center, New York, NY, USA
fCorresponding Author: Adejoke Johnson, Department of Internal Medicine, Jacobi Medical Center/North Central Bronx Hospital, Bronx, NY 10467, USA
Manuscript submitted April 12, 2024, accepted April 24, 2024, published online May 20, 2024
Short title: CTD Impact on Colorectal Surgery
doi: https://doi.org/10.14740/jcs476
| Abstract | ▴Top |
Background: Colorectal surgery poses significant risks, especially in individuals who smoke or have pre-existing conditions such as heart disease, diabetes, or obesity. However, there is a notable gap in understanding the inpatient outcomes for individuals with comorbid connective tissue disease (CTD) undergoing colorectal surgery. This study aimed to address this knowledge gap by analyzing data from the National Inpatient Sample (NIS) to evaluate these outcomes.
Methods: Utilizing the extensive NIS database covering 2016 to 2020, we conducted a retrospective analysis of colorectal surgery patients with CTD, identified through the International Classification of Diseases, 10th Revision. Primary outcomes included in-hospital mortality, while secondary outcomes encompassed postoperative abdominal complications, acute kidney injury (AKI), acute respiratory failure (ARF), sepsis, pneumonia, blood transfusion, mechanical ventilator use, and healthcare utilization. Employing STATA software, we utilized multivariate logistic and linear regression analyses to adjust for confounders.
Results: Among 19,274 colorectal surgery patients with CTD, the average age was 67.1 years, with a higher proportion of females. Patients with CTD exhibited a higher in-hospital mortality rate (6.31% vs. 4.14%) with an adjusted odds ratio of 1.55 (P ≤ 0.001). Patients with CTD had a higher likelihood of developing complications such as postoperative abdominal complications, ARF, AKI, sepsis, mechanical ventilator use, and blood transfusions.
Conclusion: Patients with CTD undergoing colorectal surgery face an elevated risk of in-hospital mortality and postoperative complications compared to those without CTD. This underscores the critical importance of integrating CTD into preoperative risk assessment and care planning for individuals undergoing colorectal surgery.
Keywords: Colorectal surgery; Connective tissue disease; National Inpatient Sample
| Introduction | ▴Top |
Connective tissue diseases (CTDs) represent a diverse group of autoimmune conditions with systemic manifestations, including gastrointestinal (GI) involvement. The severity of GI symptoms can range from mild to life-threatening in CTD patients [1]. CTDs can cause GI bleeding from various causes, such as vasculitis-induced mucosal injury, medication-related effects, or autoimmune-induced coagulopathy [2, 3]. Mesenteric vasculitis, though relatively uncommon, presents as a severe complication of CTDs, predisposing patients to bowel ischemia, infarction, and perforation [4]. Additionally, CTD patients are more prone to diverticular diseases [5], which may require surgical intervention. Colorectal surgery is pivotal in managing GI complications that are unresponsive to medical therapy or pose imminent threats to patient well-being. However, these surgeries come with their risks despite being a definitive treatment for conditions such as bowel perforation and refractory bleeding.
A retrospective analysis of single-hospital data spanning 7 years (2000 - 2006) revealed a 30-day mortality rate of 4.3% among patients undergoing colorectal resection [6], underscoring the gravity of surgical interventions in this context. However, the risks and outcomes associated with colorectal surgery in CTD patients still need to be better understood.
Our study aimed to bridge this gap by comprehensively elucidating the patient characteristics and outcomes associated with colorectal surgery in patients with CTDs compared to those without CTDs. By systematically analyzing a range of parameters, including mortality rates, postoperative complications, and healthcare utilization metrics, we sought to provide a nuanced understanding of the impact of CTDs on colorectal surgery outcomes.
| Materials and Methods | ▴Top |
This analysis was based on the National Inpatient Sample (NIS) database, part of the Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP). The NIS database is the largest inpatient care database in the USA. It consists of billing information hospitals send to state-wide data organizations in the USA. The NIS encompasses patients with various types of insurance, including Medicare, Medicaid, private insurance, or those without insurance. For Medicare, the NIS database has information on Medicare Advantage patients, who are often left out of Medicare claims data but make up 30% of Medicare benefit recipients. The NIS database has more than 100 clinical data elements from about 7 million unweighted hospitalizations annually, which is about 20% of all hospital admissions in the United States [7]. Therefore, it is crucial to follow proper methodological standards when forming subgroups and conducting analyses. For this study, we used data from 2016 to 2020, the most recent data available. This dataset is weighted to obtain national estimates.
The databases are coded using the International Classification of Diseases, 10th Revision, and Clinical Modification/Procedure Coding System (ICD-10-CM/PCS). The NIS divides diagnoses into one principal and one secondary diagnosis. A principal diagnosis is the main ICD-10 code (DX1) for the hospitalization. Secondary diagnoses are any ICD-10 code (DX2 to DX40) other than the principal diagnosis. This study was exempt from requiring Institutional Review Board approval, as it contains de-identified, publicly available data. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Utilizing the comprehensive NIS 2016 - 2020 datasets, we gathered demographic data and clinical outcomes for all adult colorectal surgery patients. The sample size for this study was determined based on the number of patients who underwent colorectal surgery and the number of patients with CTDs.
We conducted a retrospective analysis, identifying individuals aged 18 and older with a principal diagnosis of undergoing colorectal surgery and a secondary diagnosis of comorbid CTDs, encompassing conditions such as systemic lupus erythematosus (SLE), rheumatoid arthritis, scleroderma, Sjogren syndrome, inflammatory myositis, mixed CTD, giant cell arteritis, polymyalgia rheumatica, and psoriasis. This amalgamation of CTDs was systematically defined using the ICD-10-CM/PCS coding system (Supplementary Material 1, www.currentsurgery.org).
To ensure a thorough comparative analysis, we divided the cohort into two groups: one comprising individuals with CTDs who underwent colorectal surgery (colectomy, anastomosis, or colostomy), and the other composed of patients who underwent colorectal surgery without CTDs. Notably, individuals below age 18 and those with documented COVID-19 infection were excluded from both groups. This strategic exclusion was implemented to mitigate potential confounding factors related to age and the impact of COVID-19, ensuring a more focused investigation into the association between colorectal surgery and CTD.
Baseline characteristics considered encompassed patient sociodemographic and hospital characteristics, including age, race, gender, and medical conditions during admissions, including diabetes mellitus (DM), cigarette smoking, hypertension (HTN), chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), myocardial infarction, liver cirrhosis, dementia, and malignancy. Patients were also characterized based on sociodemographics such as primary payer, mean household income by quartile, disposition, hospital bed size, hospital location, and hospital teaching status, which were included in the database.
Outcome measures
The primary outcome was analyzing in-hospital mortality in patients with CTD. Secondary outcomes included the rate of post-abdominal surgery complications, acute kidney injury (AKI), acute respiratory failure (ARF), pulmonary embolism, sepsis, pneumonia, mechanical ventilator use, and blood transfusion. We also compared mean length of stay (LOS), mean total hospital charges (THC), and transfer to another acute care hospital.
Statistical analysis
Considering the complex survey design and clustering, we conducted our analyses using Stata/MP 17.0 (Stata Corp., College Station, TX). Because NIS represents a 20% stratified random sample of US hospitals, analyses were performed using hospital-level discharge weights provided by the NIS to obtain national estimates of total inpatient hospitalizations. Univariate logistic regression analysis was used to calculate unadjusted odds ratios (ORs) for the primary and secondary outcomes. Multivariate logistic regression analysis was used to adjust for potential confounders, which were hospital-level confounders. A second logistic regression model was built using only variables associated with the outcome of interest on univariate regression analysis at P < 0.2. Proportions were compared using the Fisher’s exact test, and continuous variables were compared using the Student’s t-test. All P values were two-sided, with 0.05 as the threshold for statistical significance. Logistic regression models were generated to identify the independent multivariate predictors and are reported as adjusted odds ratio (aOR) with 95% confidence intervals (CIs). Patients with missing information for any variables in the regression analyses were excluded.
| Results | ▴Top |
Patient and hospital characteristics
Out of the 678,778 patients who underwent colorectal surgery, 19,274 were diagnosed with CTDs. The patients who had both colorectal surgery and CTD were typically older, with a mean age of 67.1 years compared to 63.3 years in those without CTD. Furthermore, a significantly higher percentage of females was observed in the CTD group (71.91%) compared to males (52.74%), while males constituted the majority (47.26%) in the non-CTD group. Among CTD patients who experienced GI bleeding, most were of White ethnicity (81.1%).
The distribution of comorbidities differed between the two cohorts. Patients with CTD and GI bleeding exhibited a higher prevalence of comorbidities such as HTN, CKD, COPD, smoking history, CHF, and myocardial infarction. Additionally, most of these patients were covered by Medicare insurance and were more likely to seek care at urban teaching hospitals (Table 1).
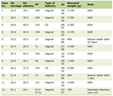 Click to view | Table 1. Patient and Hospital Characteristics |
Outcomes
Primary outcome: in-hospital mortality
Patients who underwent colorectal surgery and had comorbid CTD exhibited a higher in-hospital mortality rate of 6.31%, in contrast to the 4.14% mortality rate observed in non-CTD patients (Table 2). This difference in mortality rate was statistically significant, and results persisted after adjusting for critical factors such as demographics, hospital characteristics, and comorbidities. The aOR was 1.46 (95% CI: 1.27 - 1.69, P ≤ 0.001).
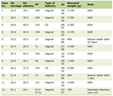 Click to view | Table 2. Outcomes of Colorectal Surgery in Patients With Coexisting CTDs |
Secondary outcomes
Patients with CTD who underwent colorectal surgery had a higher rate of post-abdominal complications (25.45 vs. 22.51, OR: 1.18, 95% CI: 1.09 - 1.27). The rate of AKI and ARF was higher in patients with underlying CTD (OR: 1.17, 95% CI: 1.07 - 1.29 and OR 1.24, 95% CI: 1.09 - 1.40, respectively). Within the complications observed, sepsis presented predominantly in patients with CTD with an aOR of 1.32 (95% CI: 1.19 - 1.46), as well as the need for ventilator use (OR: 1.2, 95% CI: 1.09 - 1.39) (Table 2). There were significant differences in LOS (OR: 0.576, 95% CI: 0.2358 - 0.9189), and transfer to other facilities (OR: 1.26, 95% CI: 1.16 - 1.37) compared to patients without CTDs (Table 2).
| Discussion | ▴Top |
Our analysis revealed that patients with CTDs who underwent colorectal surgery exhibited a significantly elevated rate of in-hospital mortality compared to their counterparts without CTDs (6.31% vs. 4.14%, P ≤ 0.001). This finding resonates with findings from a 2019 retrospective study, which aimed to identify prognostic factors associated with mortality following surgery for colorectal perforation [8]. The study demonstrated that cumulative survival rates in CTD patients were notably worse than those in non-CTD patients post-surgery for colorectal perforation [8]. The heightened mortality risk in CTD patients was attributed to fecal peritonitis precipitating sepsis, particularly significant given the generally immunosuppressed backgrounds of CTD patients. Our analysis also identified a higher incidence of sepsis among CTD patients during hospitalization (14.29 vs. 11.14, P ≤ 0.001), further underscoring the vulnerability of this patient population to postoperative complications and increased mortality.
Our analysis revealed that patients with CTDs undergoing colorectal surgery exhibited higher Charlson Comorbidity scores, indicating a more significant burden of concurrent conditions such as HTN, CKD, COPD, and CHF. These comorbidities are known to influence surgical outcomes and may contribute to the increased mortality observed among patients with CTD. Consistent with previous findings, a prospective study conducted in 2020 highlighted the impact of comorbidities on surgical outcomes, particularly in general surgery, where conditions such as HTN, DM, and CKD were associated with an increased risk of postoperative complications [9]. In our study, patients with CTD demonstrated significantly higher rates of postoperative complications (25.45% vs. 22.51%, P < 0.001), which may be attributed to the higher prevalence of comorbidities in this patient population.
While our analysis did not specify the type of postoperative complications, it is crucial to recognize anastomotic leak as a significant concern following colorectal surgery due to its associated morbidity and mortality [10]. Inadequate surgical site healing is one of the primary causes of anastomotic leaks [10]. CTDs are characterized by chronic inflammation and tissue fibrosis, which can impair wound-healing processes [11]. Additionally, the use of immunosuppressive medications further compromises tissue integrity, predisposing individuals to an increased risk of anastomotic leak and subsequent mortality [12]. Furthermore, our analysis identified a higher incidence of AKI, ARF requiring ventilator support, and the need for blood transfusion among CTD patients undergoing colorectal surgery. These complications can be attributed to the complexity of underlying diseases, immunosuppressive therapy, vascular involvement, and increased bleeding risk associated with CTDs.
Moreover, our analysis revealed notable demographic and clinical differences between CTD patients undergoing colorectal surgery and those without CTDs. CTD patients tended to be older and had a higher proportion of females, aligning with previous findings indicating a higher prevalence of autoimmune diseases among females and an increased risk of autoimmune disorders with advancing age.
These findings highlight the importance of careful preoperative assessment and optimization in CTD patients undergoing colorectal surgery to minimize the risk of complications and improve outcomes.
Strength and limitation
The retrospective design of our study allows for the establishment of associations but cannot imply causality. It is important to note that while ICD-10-CM codes for colorectal surgery and CTD have been previously validated and employed, variations in coding accuracy across different hospitals cannot be ruled out. Moreover, the NIS provides data on hospitalizations rather than individual patients, which means that patients hospitalized multiple times cannot be counted repeatedly. One notable observation is the overrepresentation of the white population in our study, which warrants consideration. It is essential to recognize that more severe cases and higher disease activity associated with CTD are often found in non-Caucasian populations. Therefore, further research in this specific population subset may be necessary to validate or replicate our findings.
Furthermore, the NIS dataset does not contain information on physical examinations, vital signs, laboratory values, or medications, preventing an assessment of patients’ CTDs. Despite these limitations, our study possesses several strengths. It is one of the few investigations that have delved into the outcomes of colorectal surgery in patients with CTDs. Utilizing the largest inpatient database in the USA enhances the robustness of our study. The study uses the NIS, an extensive, nationally representative database that enhances external validity. Including a diverse range of patients from different regions and healthcare settings in the USA increases the likelihood that the findings can be generalized to the broader population. Our scientific inquiry and analytical approach contribute valuable new insights to a relatively underexplored topic.
Conclusion
Our study sheds light on the intricate interplay between CTDs and colorectal surgery outcomes, revealing higher mortality rates and postoperative complications in colorectal surgery patients with CTDs compared to those without. Our findings underscore the importance of comprehensive risk stratification, considering factors such as age, gender, comorbidities, and disease severity, to tailor management approaches effectively. Furthermore, awareness of the heightened susceptibility of CTD patients to complications such as anastomotic leak, AKI, and sepsis is crucial for optimizing perioperative care and improving patient outcomes. Further research is needed to explore specific CTD subtypes and inform evidence-based guidelines. Our findings underscore the importance of multidisciplinary collaboration and patient-centered care to optimize outcomes in this complex patient population.
| Supplementary Material | ▴Top |
Suppl 1. ICD-10 Codes.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Conception and design: Adejoke Johnson. Administrative support: Khan Zinobia and Moses Bachan. Provision of study materials or patients: Adejoke Johnson. Collection and assembly of data: Ezekiel Akpan and Chukwunonso Ezeani. Data analysis and interpretation: Adejoke Johnson and Marianne Solano. Manuscript writing: all authors. Final approval of manuscript: all authors.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Cojocaru M, Cojocaru IM, Silosi I, Vrabie CD. Gastrointestinal manifestations in systemic autoimmune diseases. Maedica (Bucur). 2011;6(1):45-51.
pubmed pmc - Tian XP, Zhang X. Gastrointestinal involvement in systemic lupus erythematosus: insight into pathogenesis, diagnosis and treatment. World J Gastroenterol. 2010;16(24):2971-2977.
doi pubmed pmc - Xie F, Yun H, Bernatsky S, Curtis JR. Brief report: risk of gastrointestinal perforation among rheumatoid arthritis patients receiving tofacitinib, tocilizumab, or other biologic treatments. Arthritis Rheumatol. 2016;68(11):2612-2617.
doi pubmed pmc - Yuan S, Ye Y, Chen D, Qiu Q, Zhan Z, Lian F, Li H, et al. Lupus mesenteric vasculitis: clinical features and associated factors for the recurrence and prognosis of disease. Semin Arthritis Rheum. 2014;43(6):759-766.
doi pubmed - Broad JB, Wu Z, Clark TG, Musson D, Jaung R, Arroll B, Bissett IP, et al. Diverticulosis and nine connective tissue disorders: epidemiological support for an association. Connect Tissue Res. 2019;60(4):389-398.
doi pubmed - Visser BC, Keegan H, Martin M, Wren SM. Death after colectomy: it's later than we think. Arch Surg. 2009;144(11):1021-1027.
doi pubmed - Project HCaU. Introduction to the HCUP National Inpatient Sample (NIS). https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2016.jsp, and https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2017.jsp. Accessed January 20, 2021.
- Sugimoto K, Sakamoto K, Okazawa Y, Takahashi R, Mizukoshi K, Ro H, Kawai M, et al. Colorectal perforation in patients with connective tissue disease. Emerg Med Int. 2019;2019:5852438.
doi pubmed pmc - Dharap SB, Barbaniya P, Navgale S. Incidence and risk factors of postoperative complications in general surgery patients. Cureus. 2022;14(11):e30975.
doi pubmed pmc - Bosmans JW, Jongen AC, Bouvy ND, Derikx JP. Colorectal anastomotic healing: why the biological processes that lead to anastomotic leakage should be revealed prior to conducting intervention studies. BMC Gastroenterol. 2015;15:180.
doi pubmed pmc - Spagnolo P, Cordier JF, Cottin V. Connective tissue diseases, multimorbidity and the ageing lung. Eur Respir J. 2016;47(5):1535-1558.
doi pubmed - Hernandez PT, Paspulati RM, Shanmugan S. Diagnosis of Anastomotic Leak. Clin Colon Rectal Surg. 2021;34(6):391-399.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.
